How To Write A Soap Note
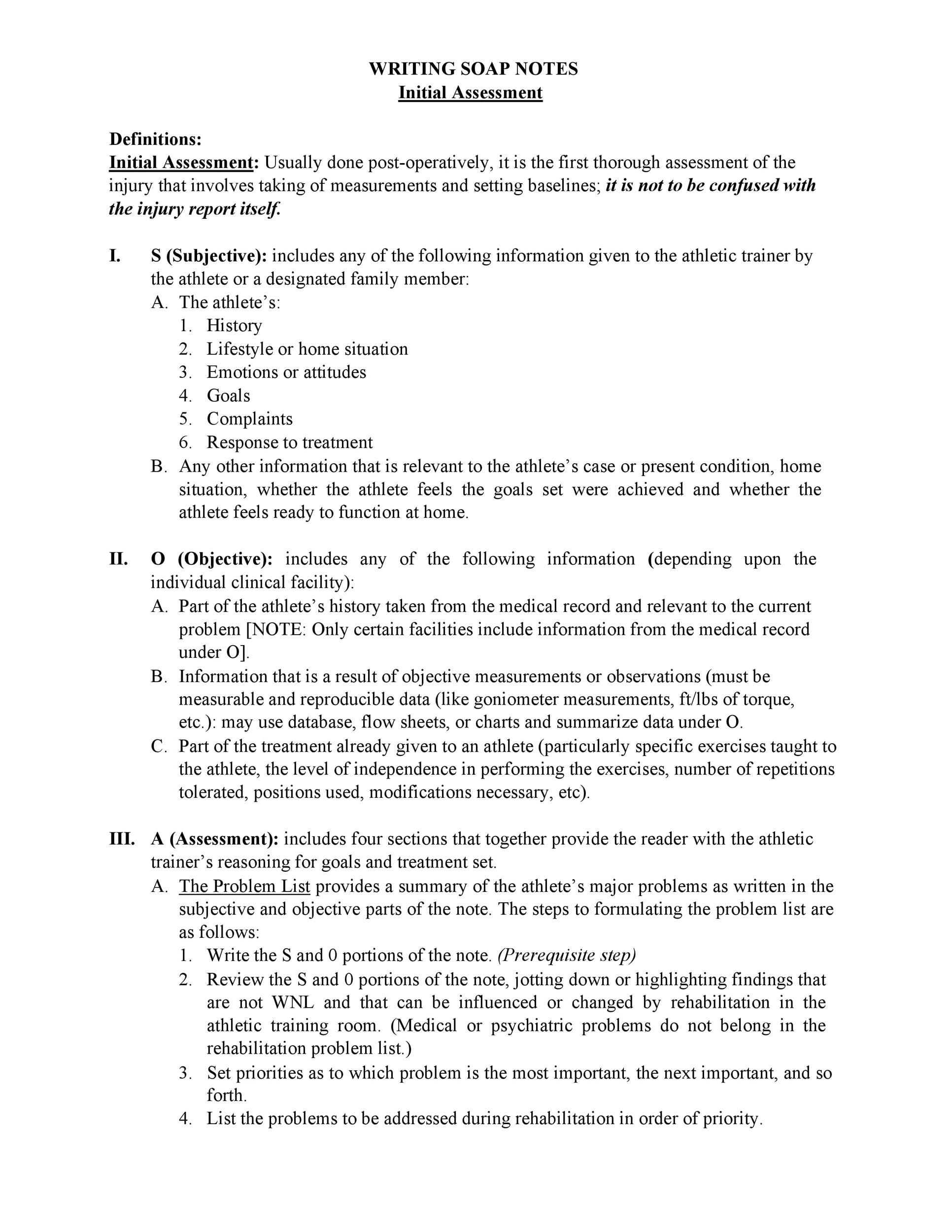
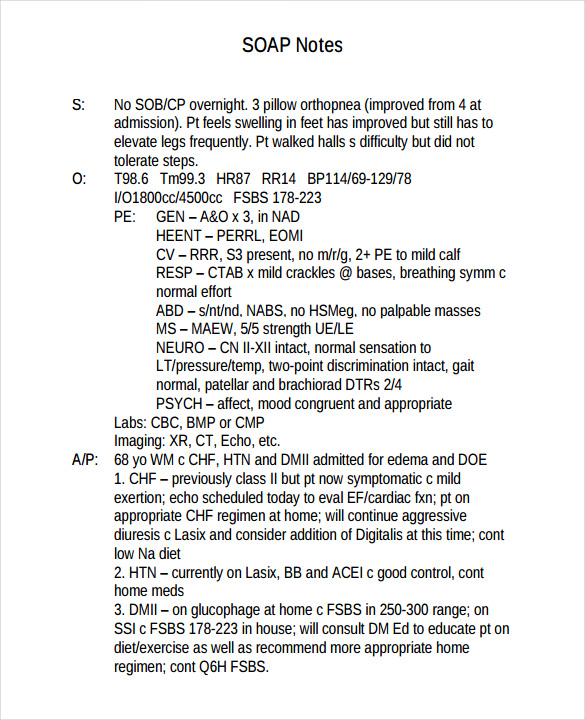
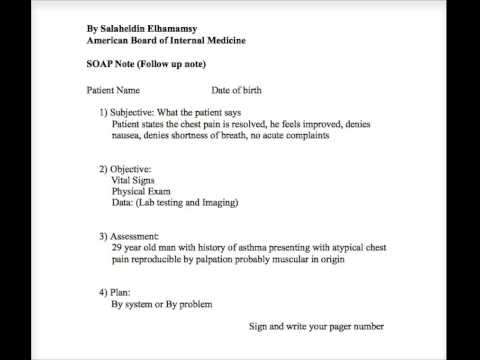
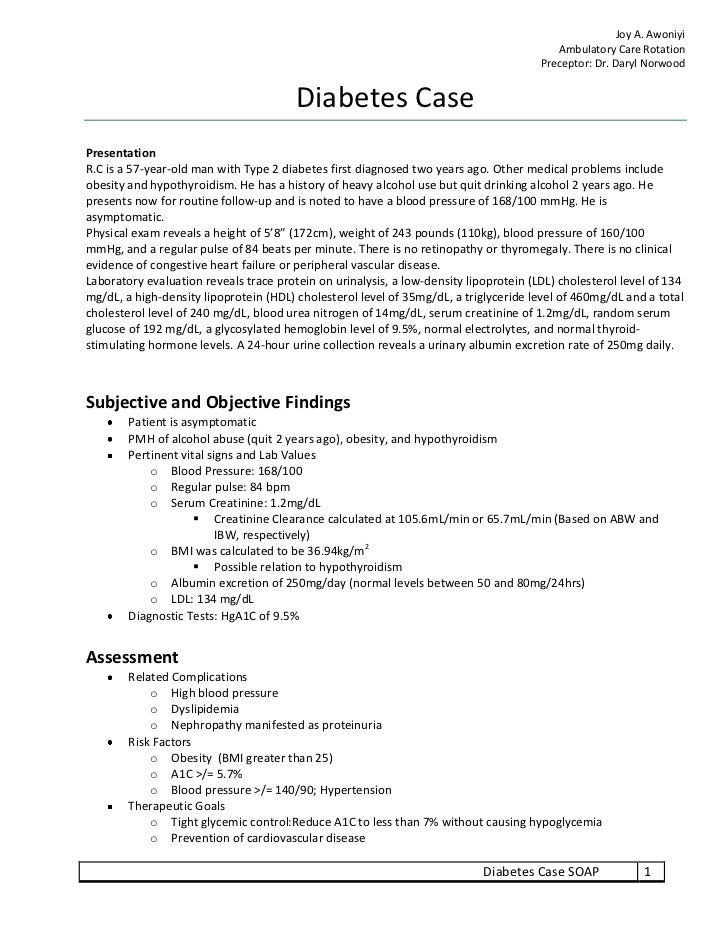
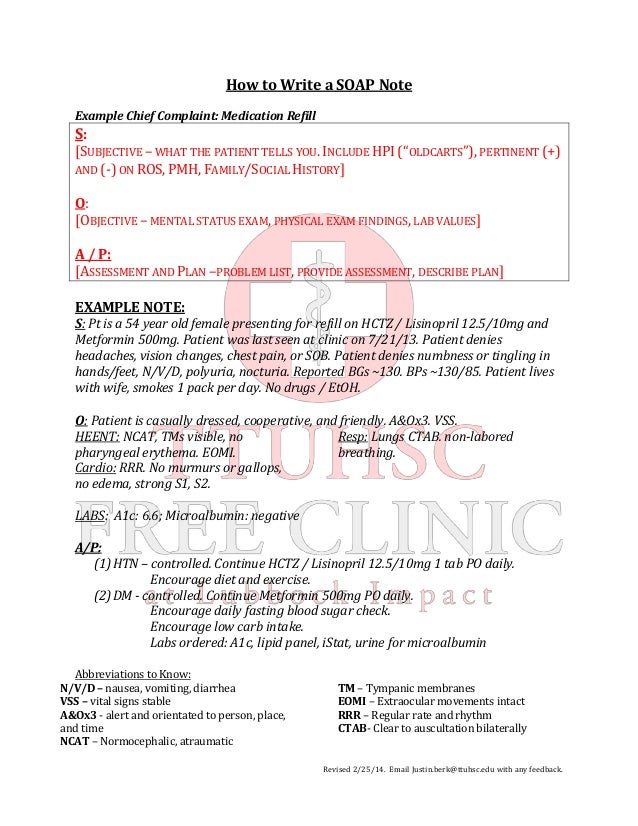
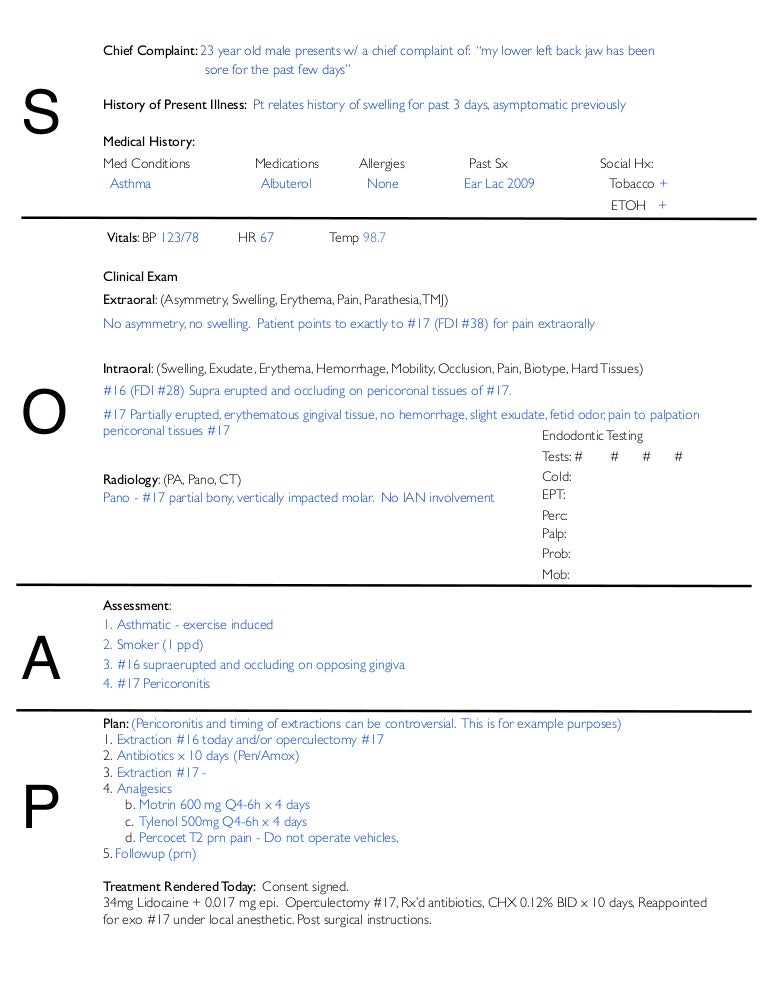
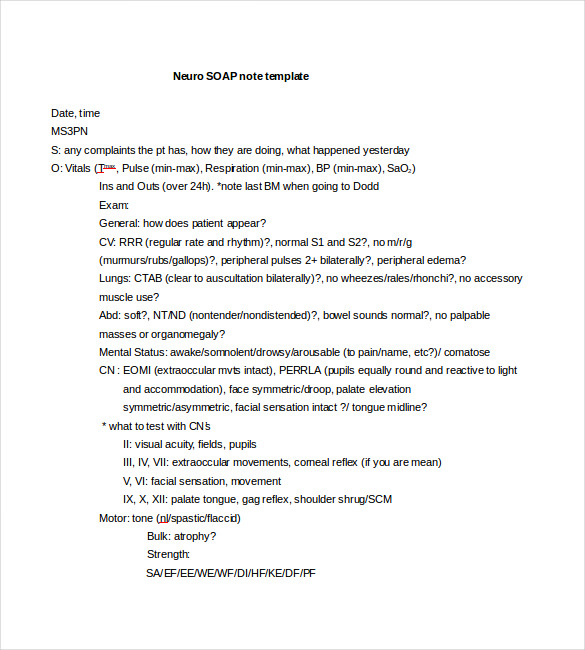
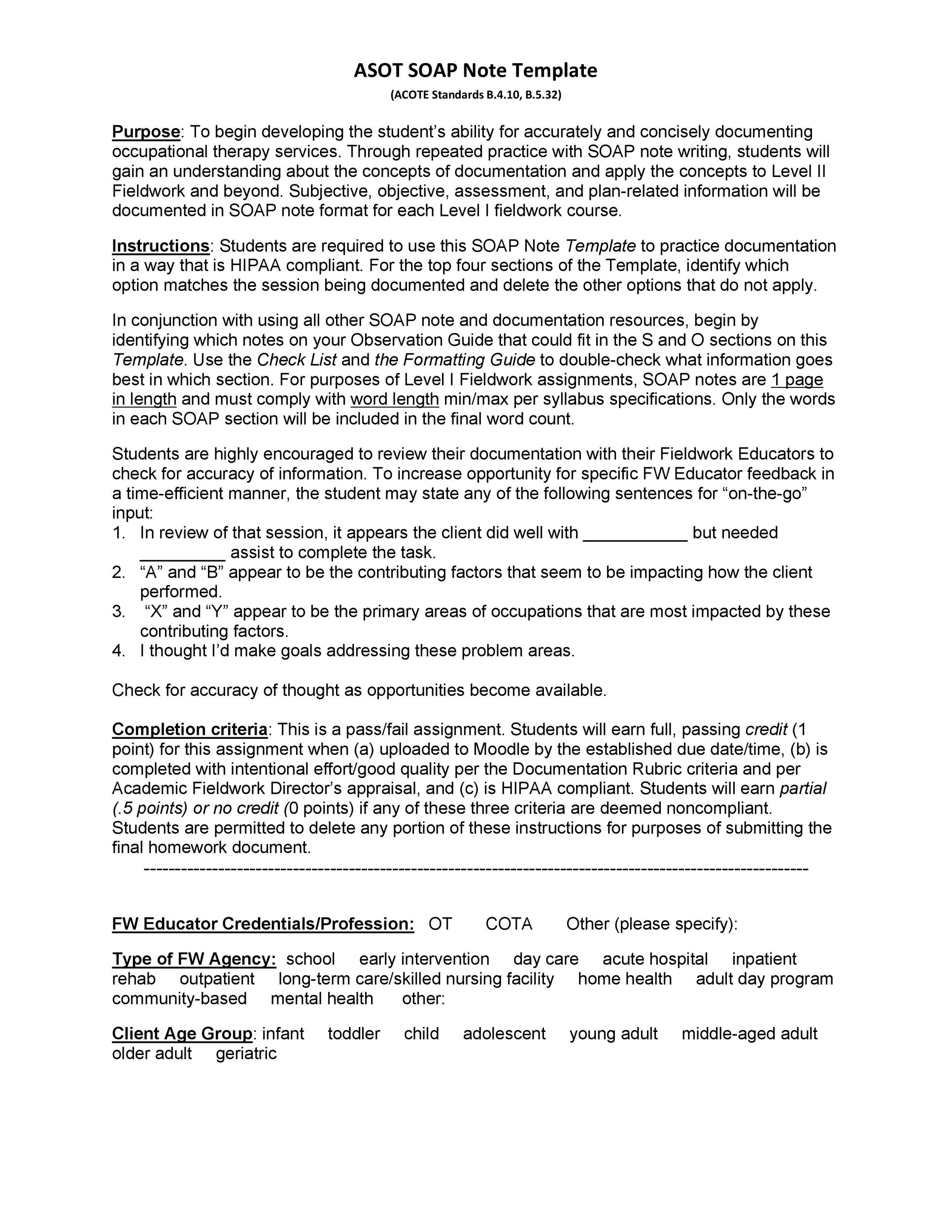
The objective portion of a soap note includes factual information.
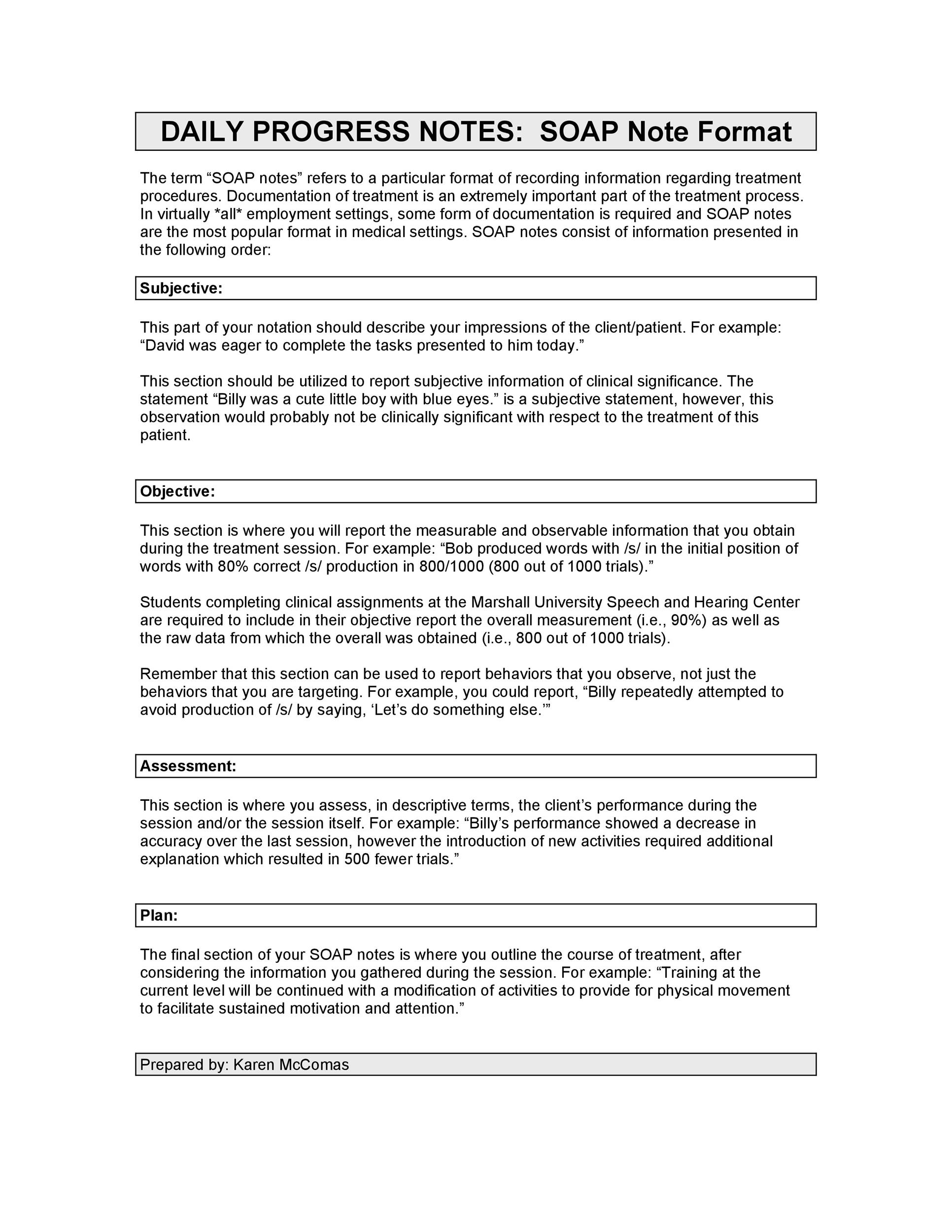
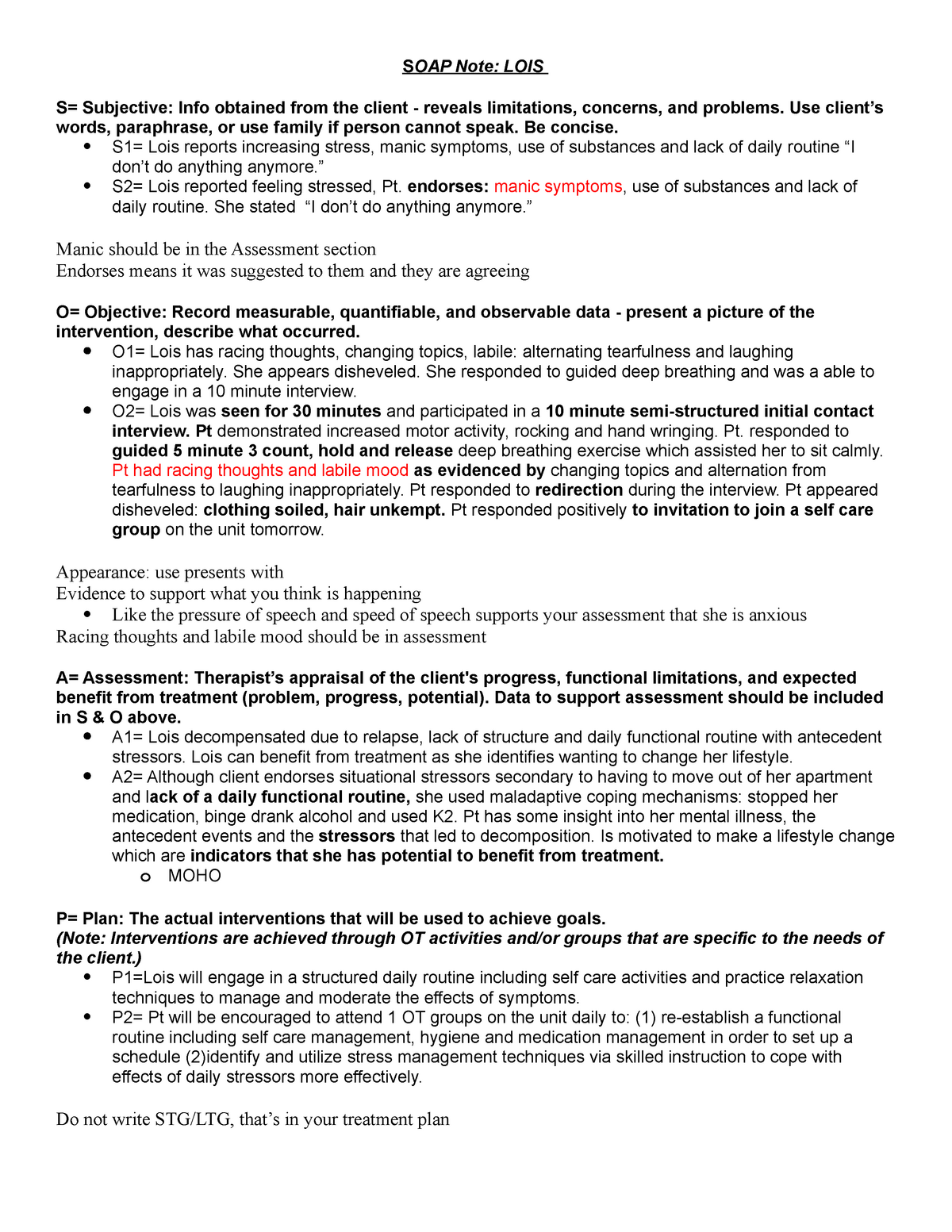
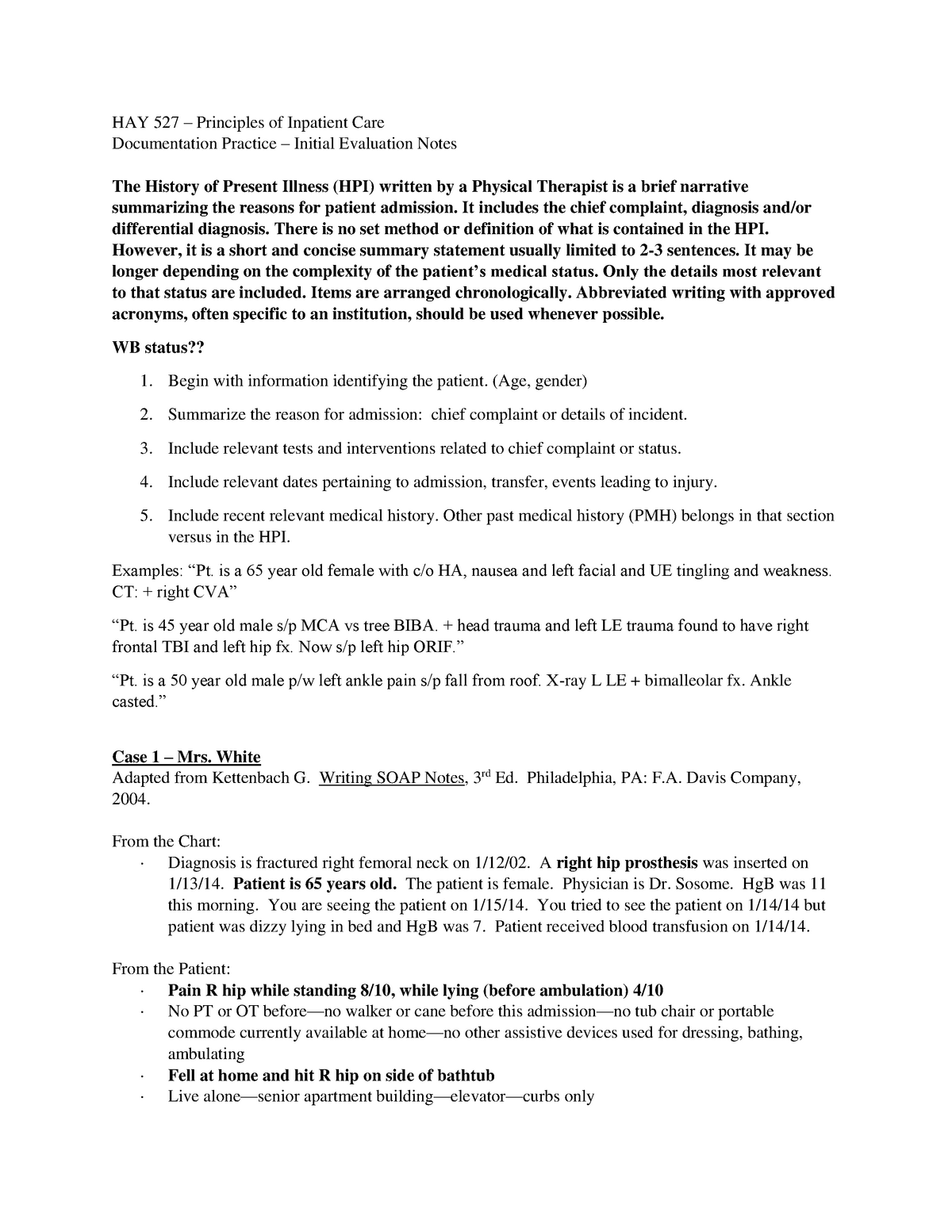
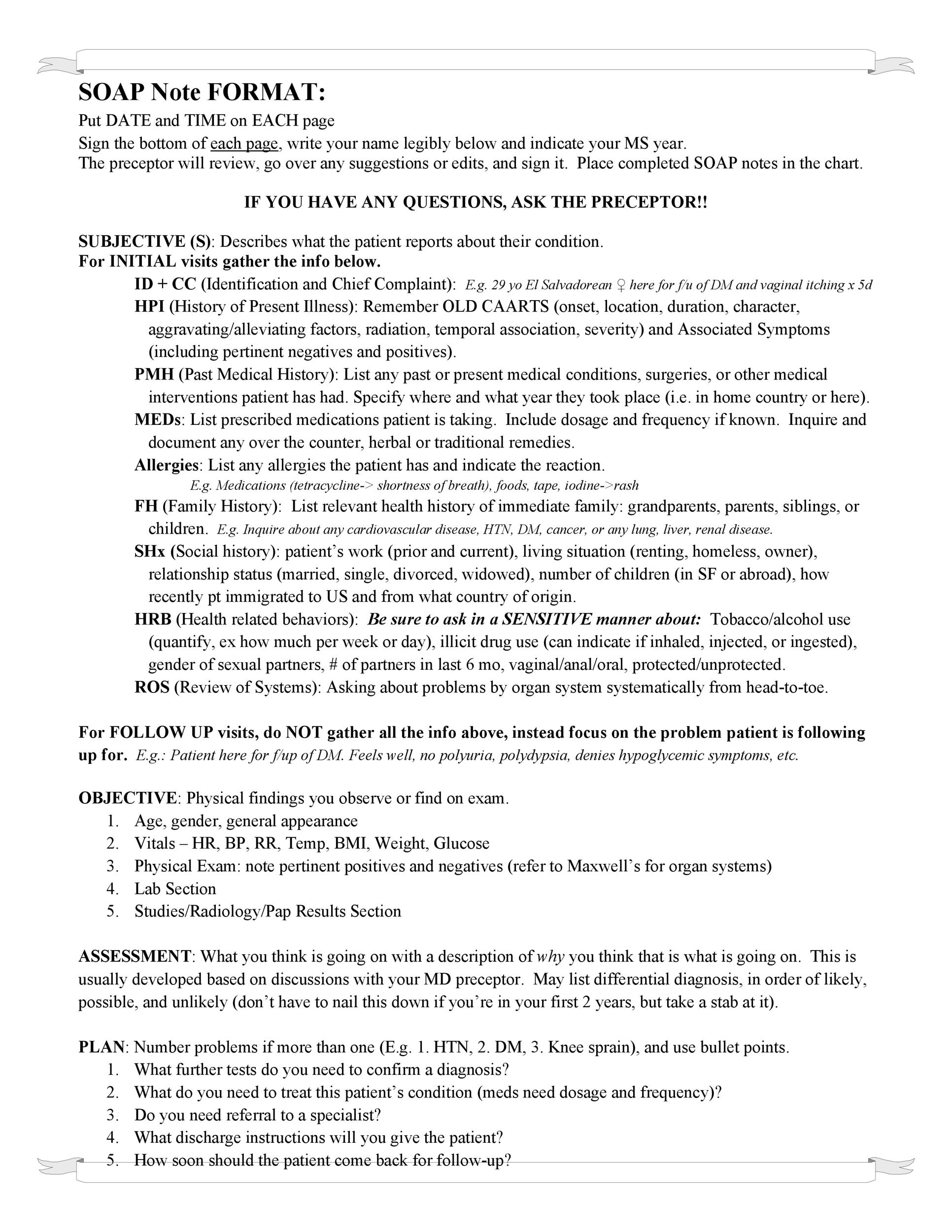
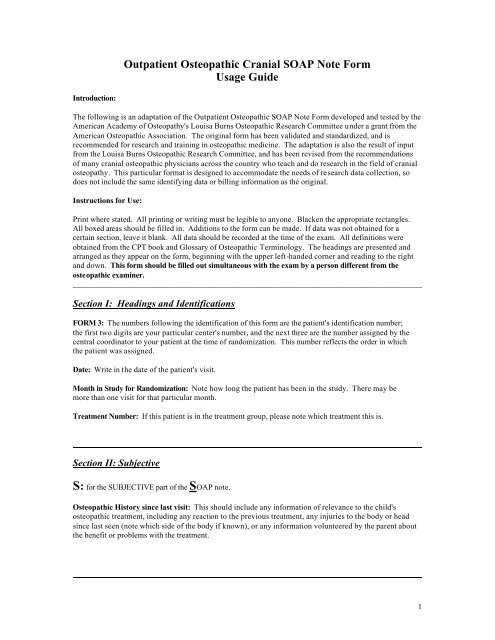
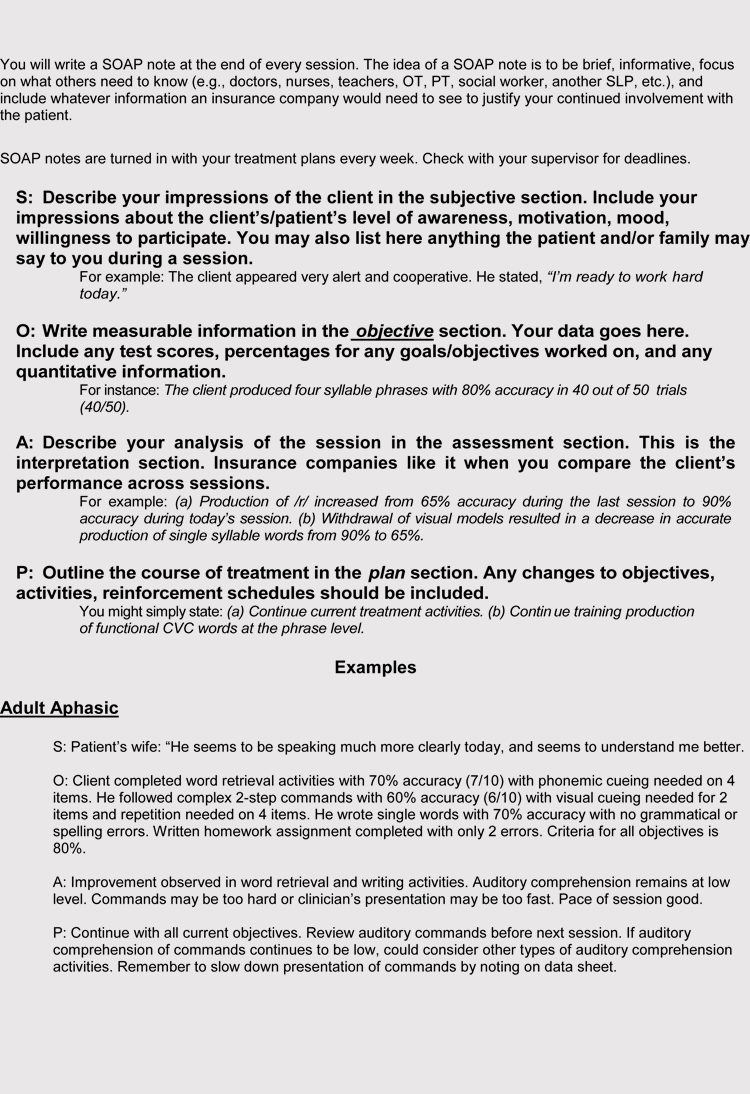
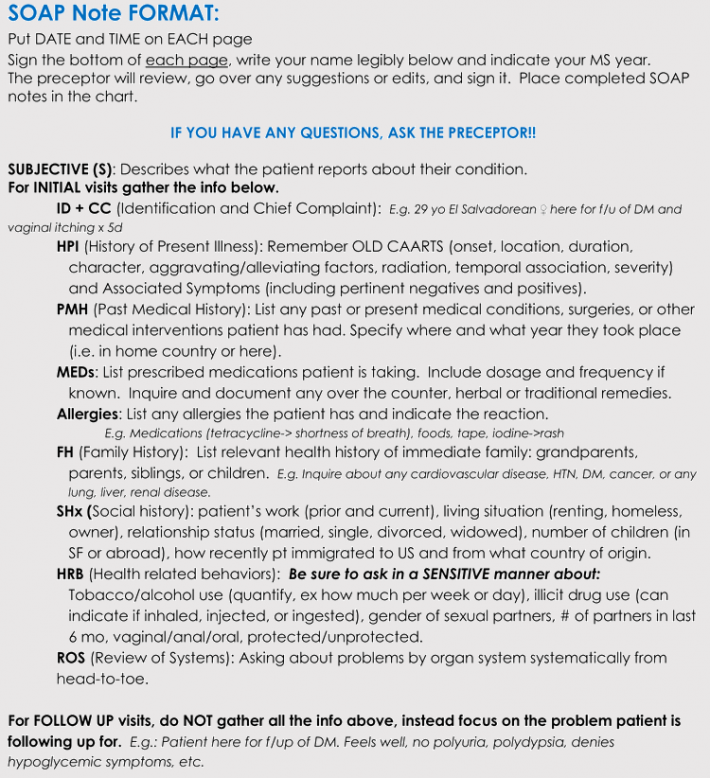
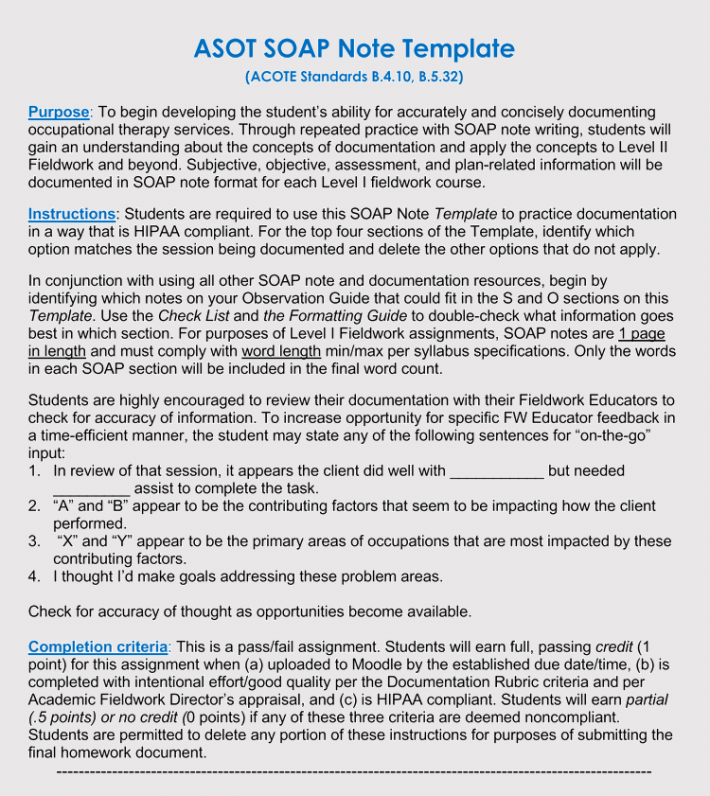
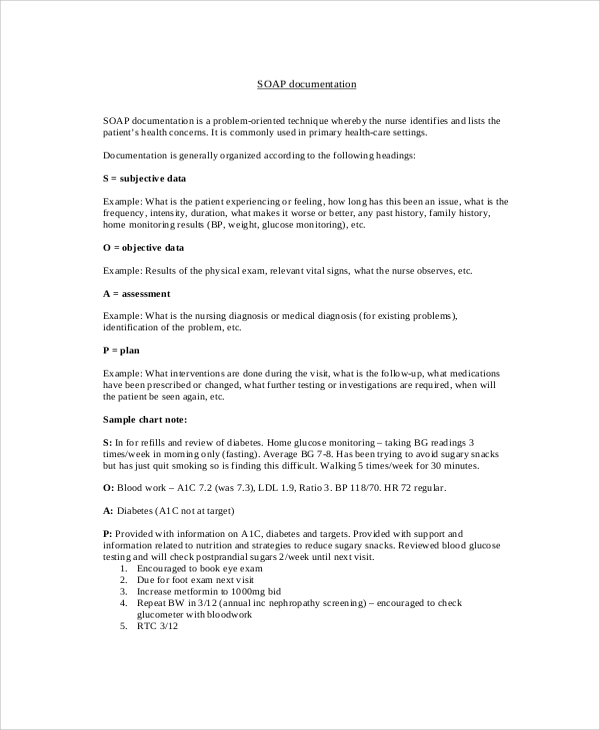
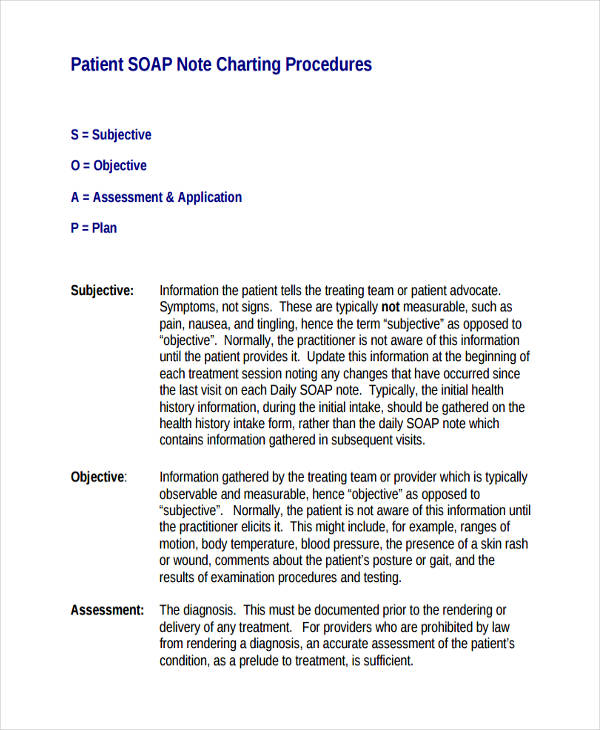
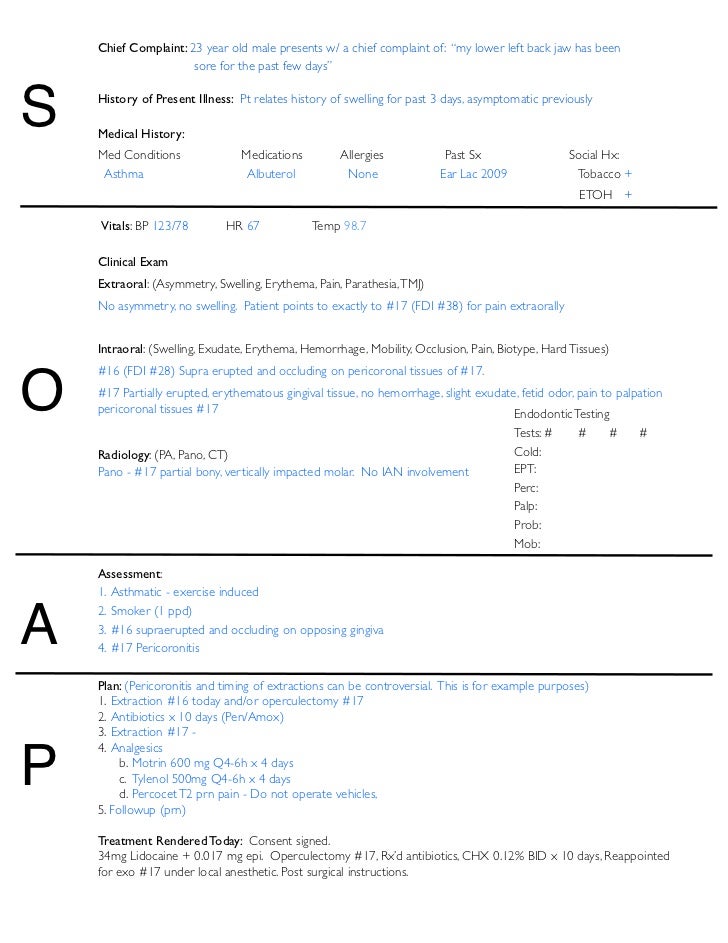
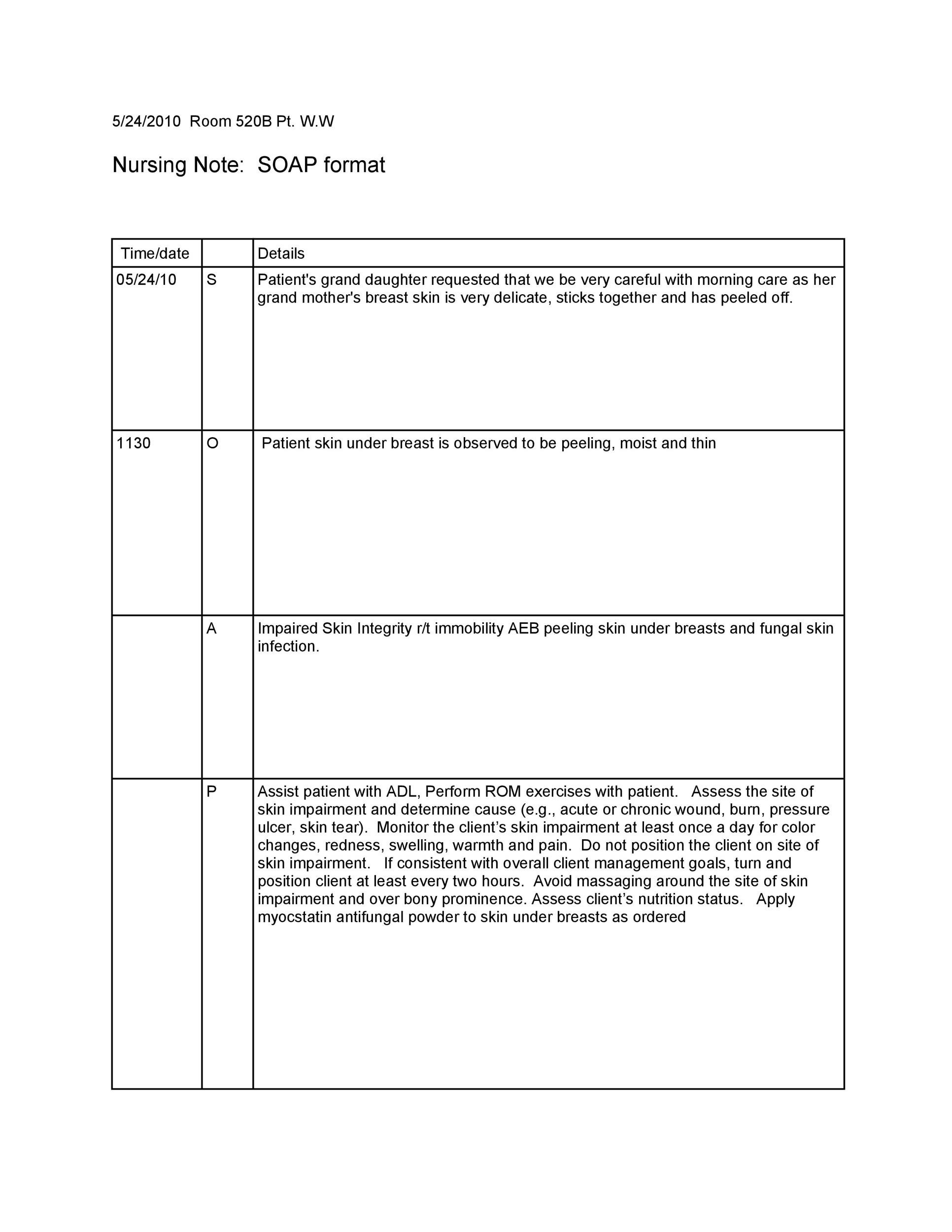
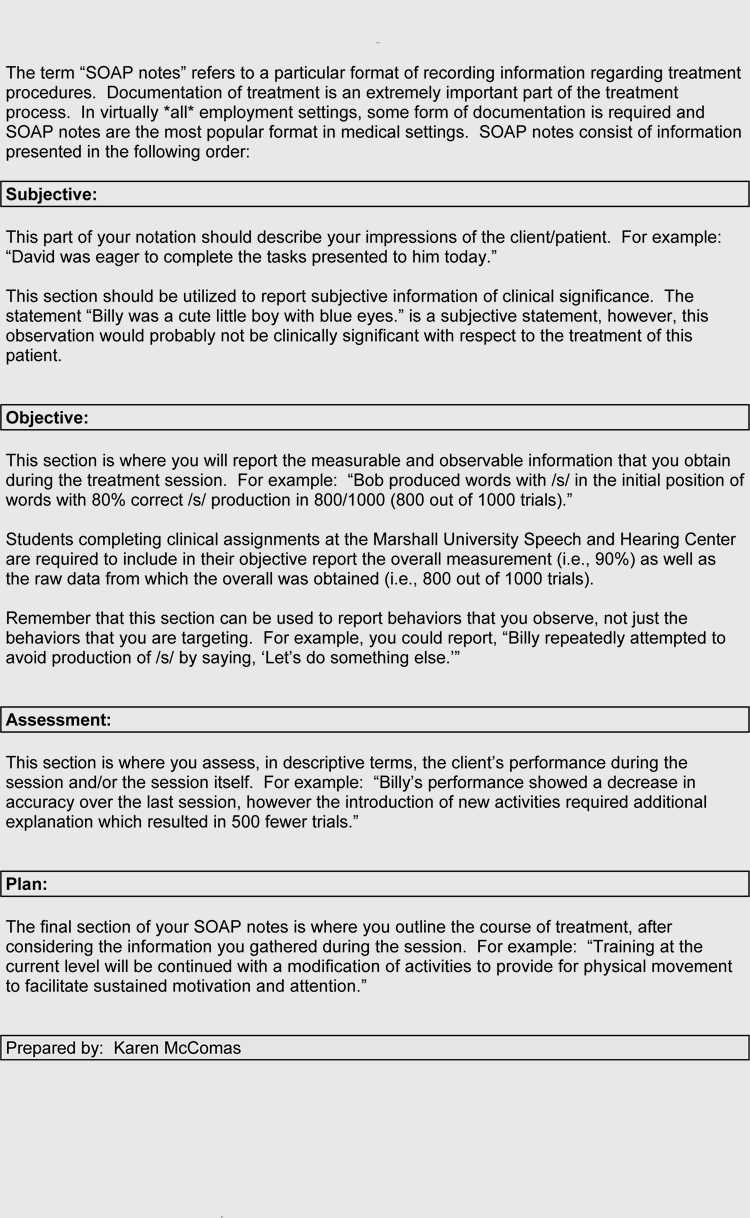
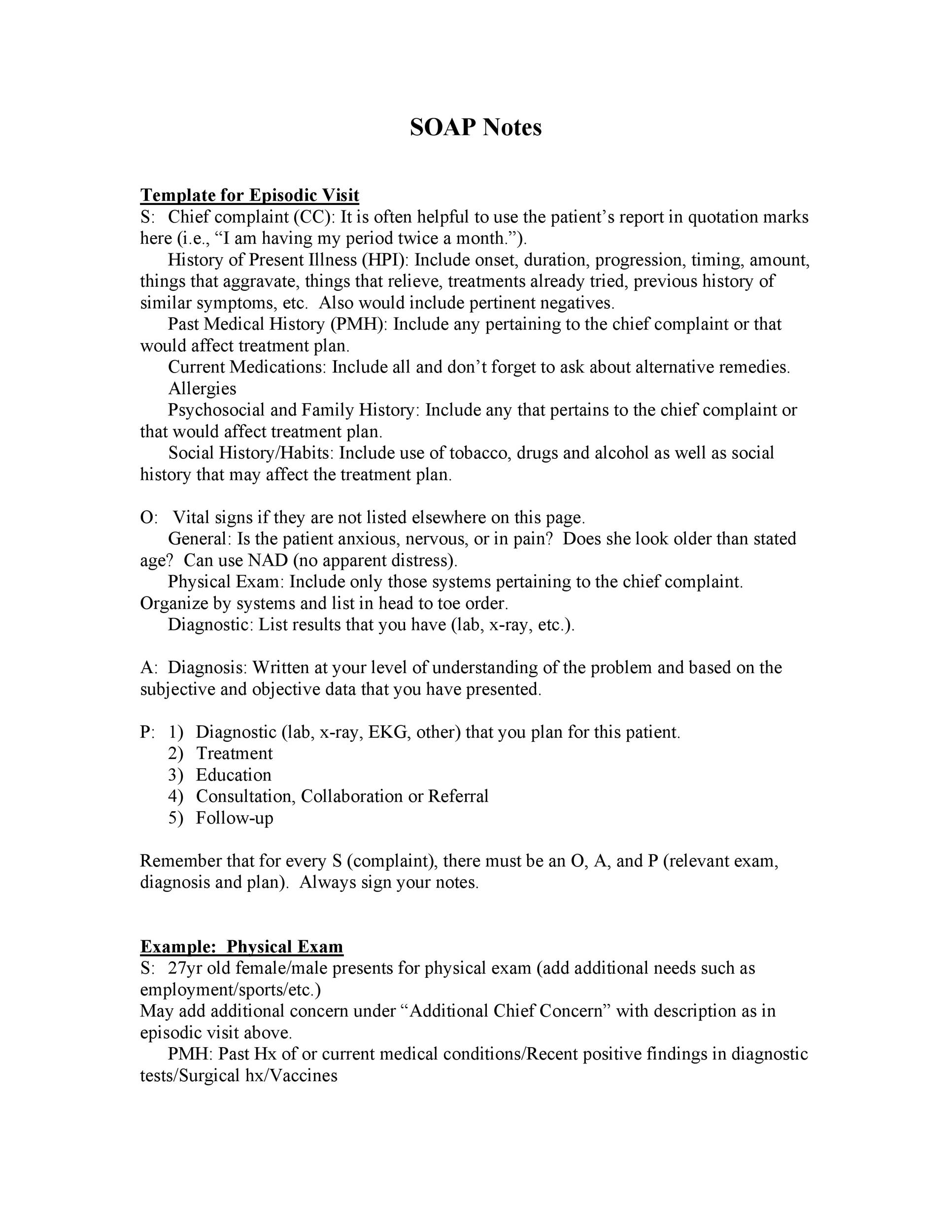
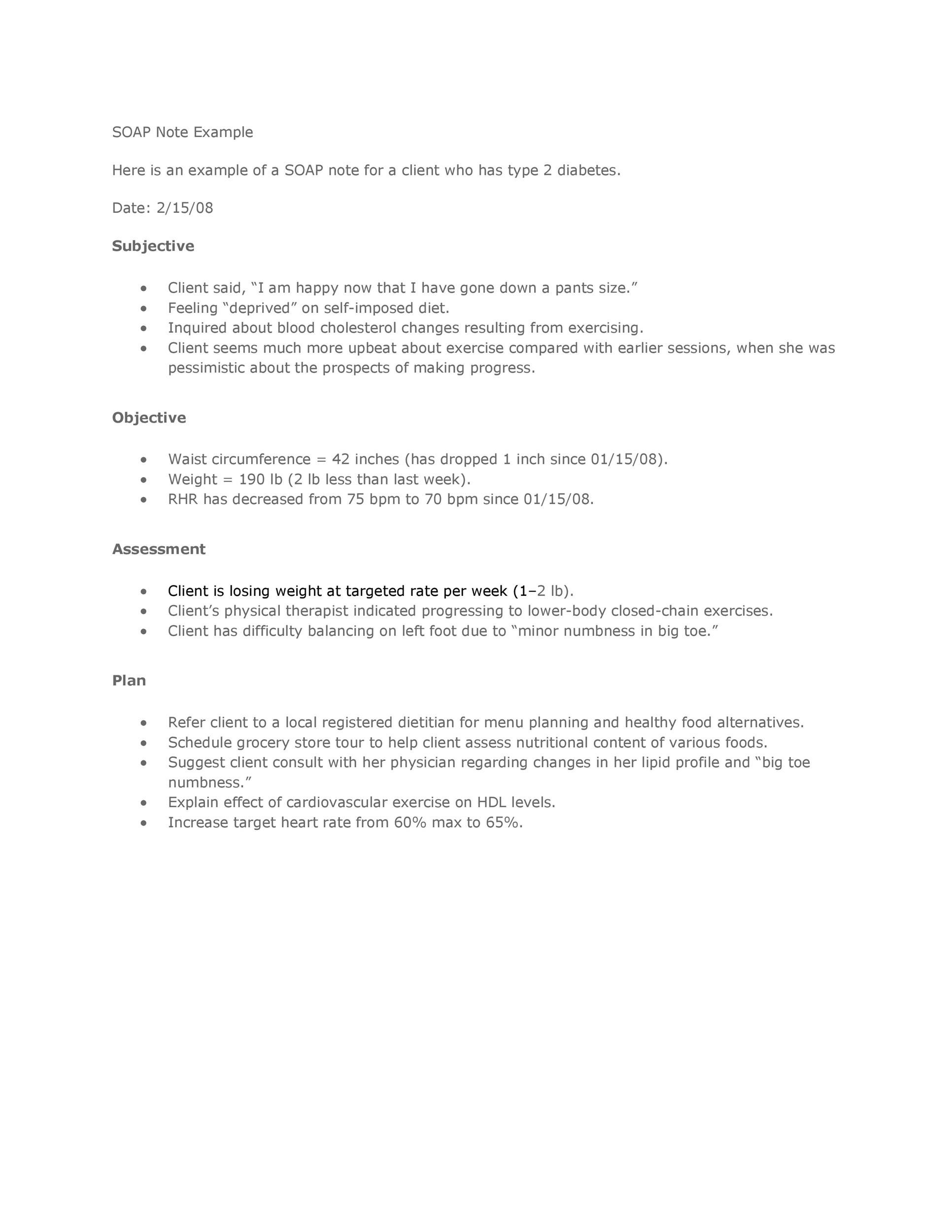
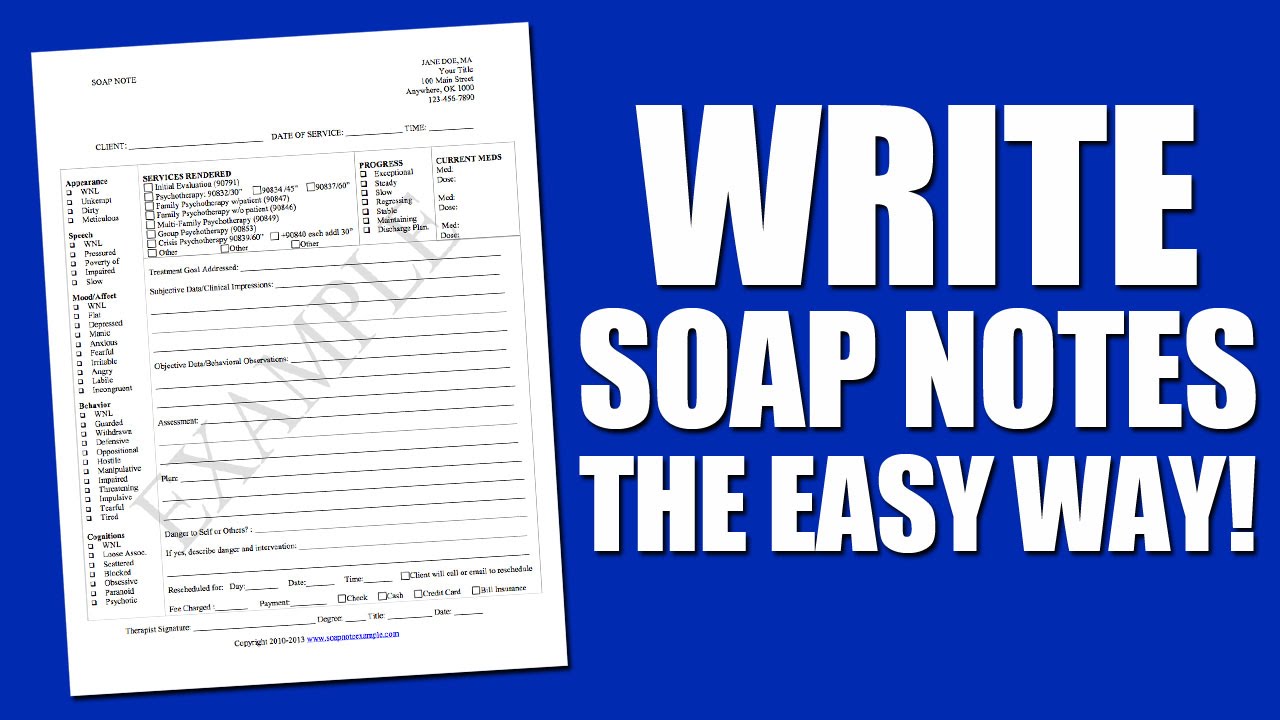
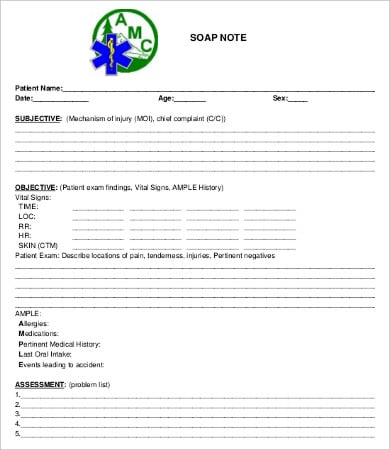
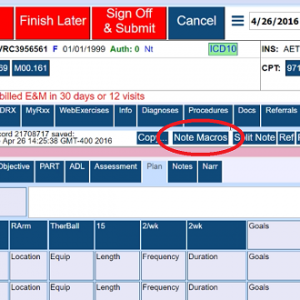
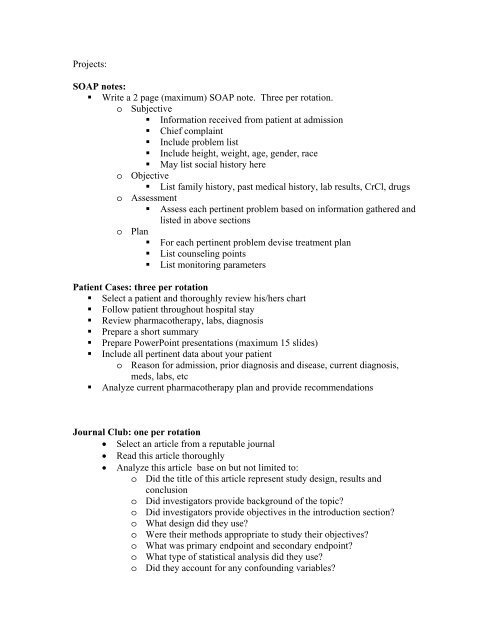
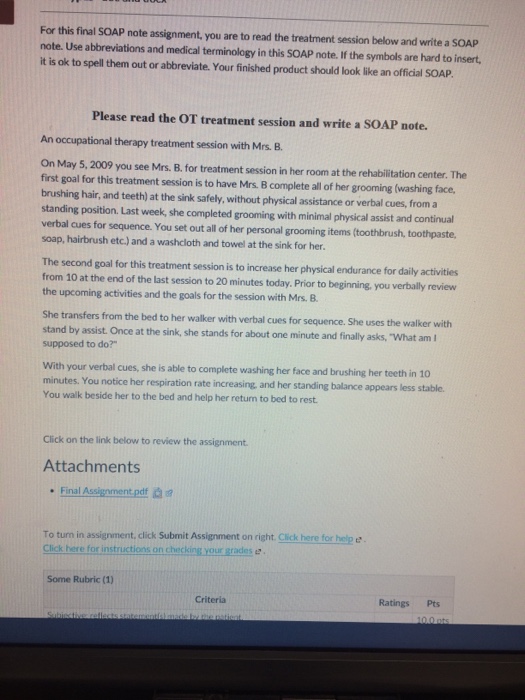
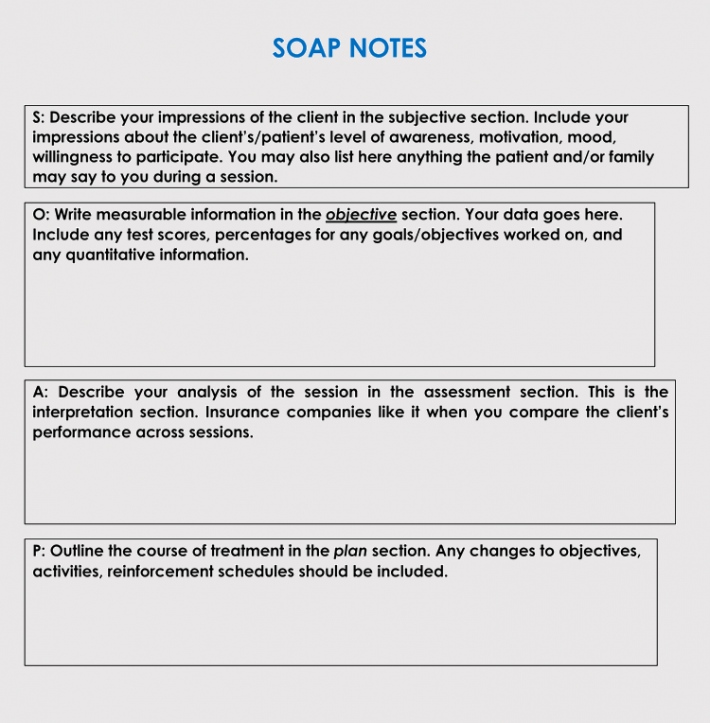
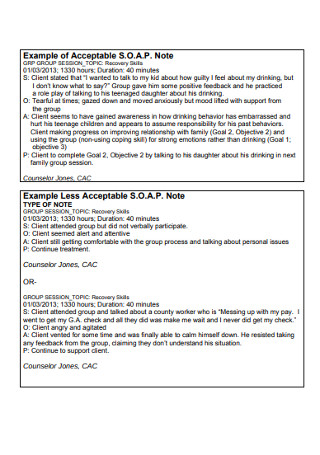
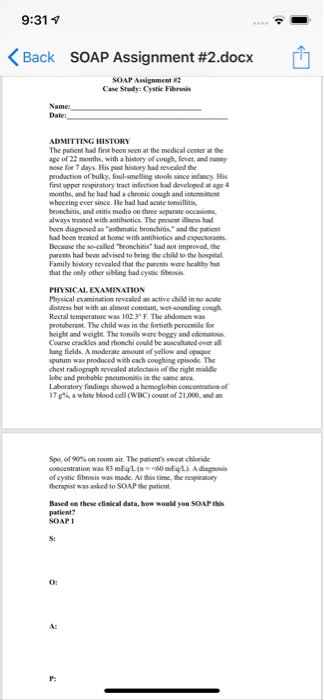
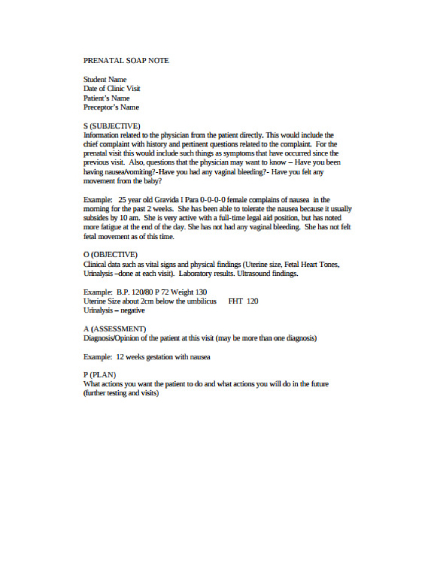
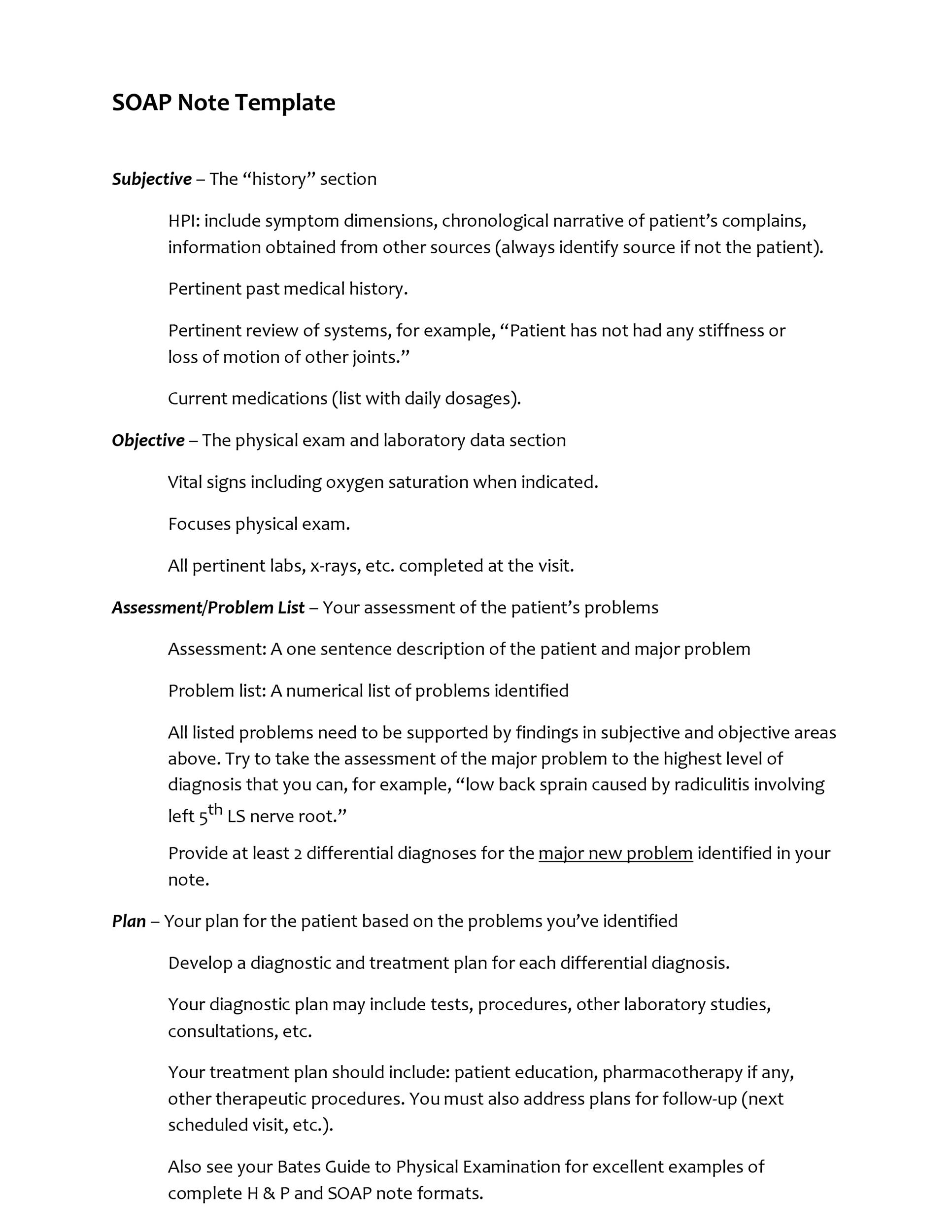
How to write a soap note. Write details down as factually as possible. Consider writing the minutes immediately youre through with the soap ie when the details are still fresh in your mind. S stands for subjective information. Make your soap note as concise as possible but make sure that the information you write will sufficiently describe the.
Write it clearly and. This area shows the patients status and facts ie. O stands for objective information. You should take personal notes for yourself that you can use to help you write soap notes.
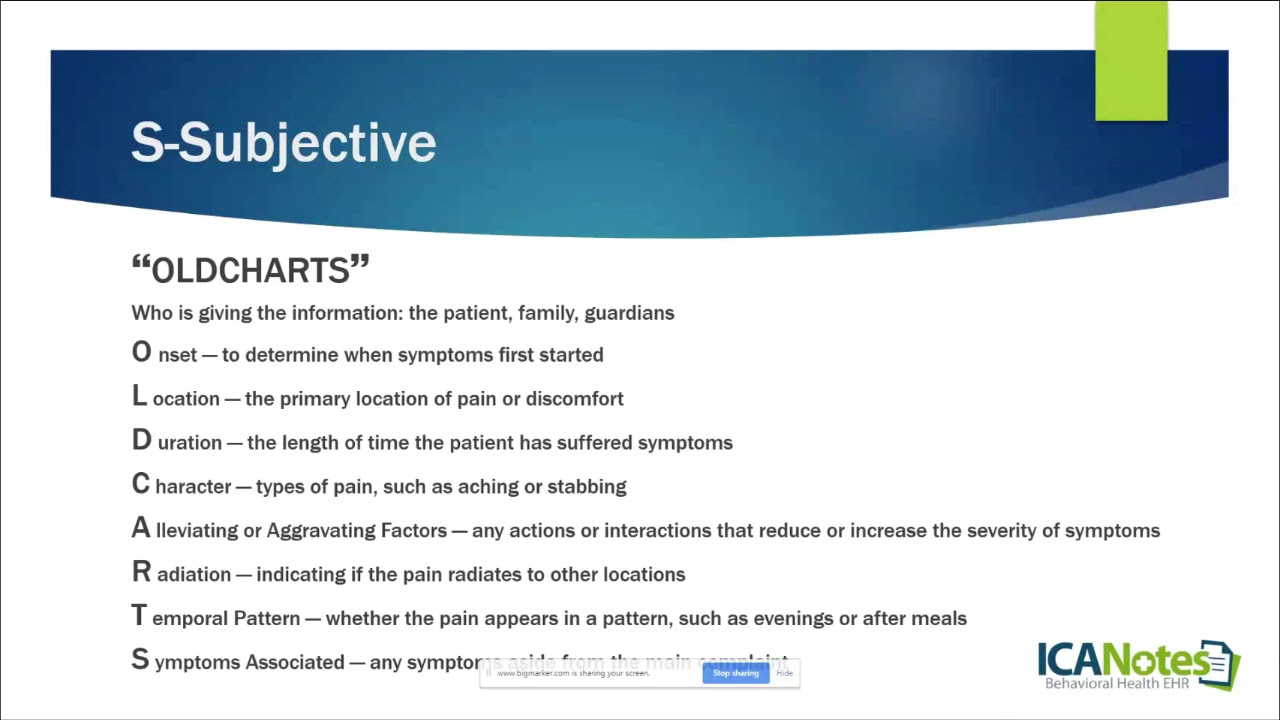
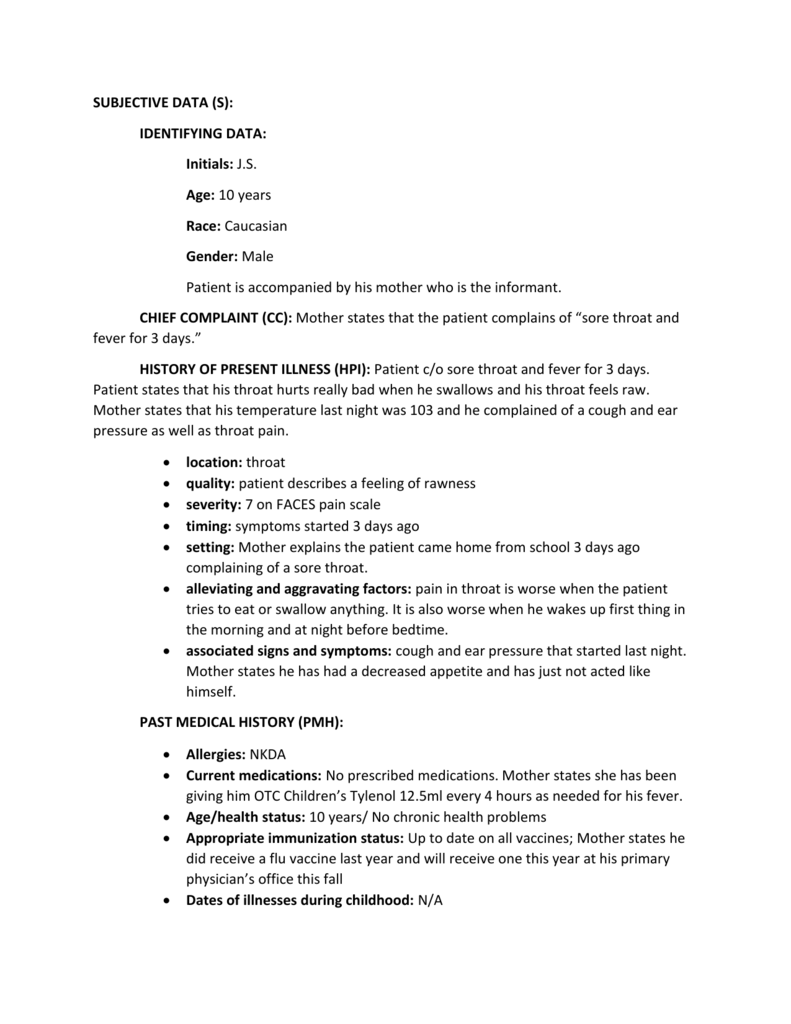
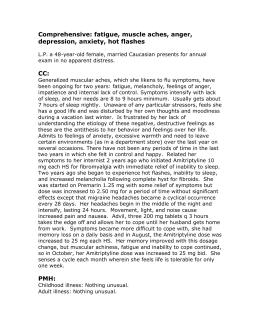
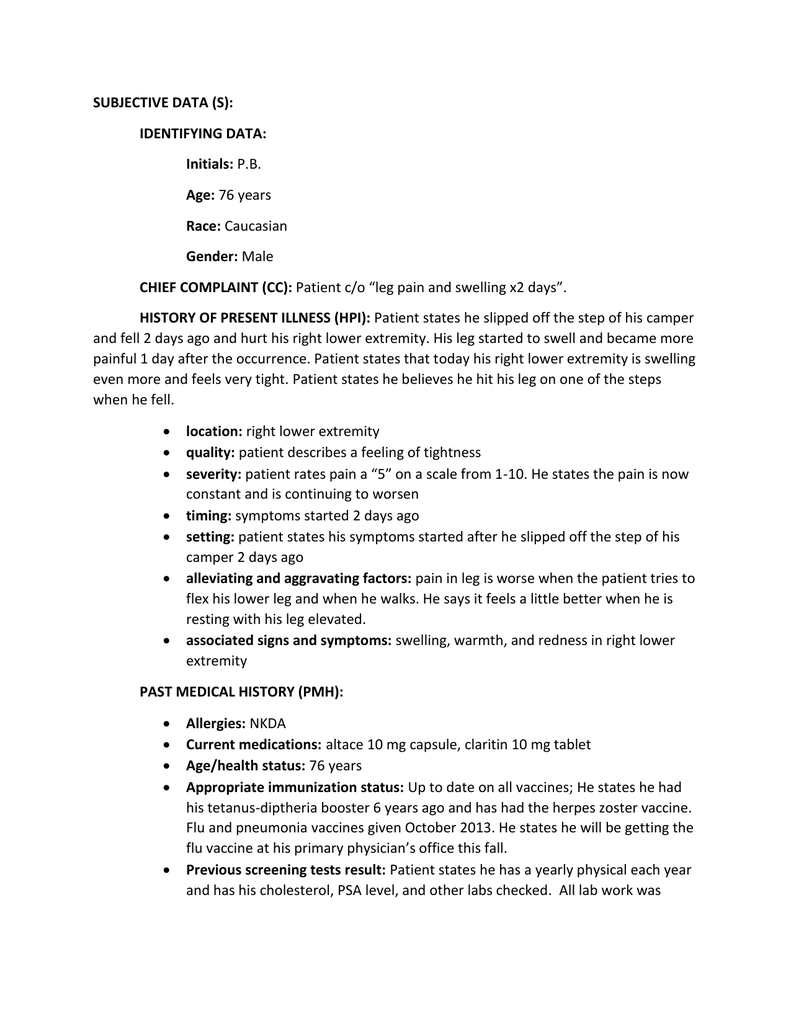
It also contains the information the patient reports to the medical practitioner. Start from the subjective followed by the objective then the. Writing soap notes while you are in the session with a patient or client. A brief statement of medical diagnose for a patients medical visit on the same day the soap note is written.
Waiting too long after your session with a client or a patient has ended. How to write soap minutes. When writing soap notes the first thing you need to do is write the subjective portion. Tips for effective soap notes.
Sample soap note for mental health therapists. It may include detailed observations about the clients appearance behavior body language and mood. After that section record the patients vital signs and anything you gather from a physical exam for the objective section. For example you might write that the client arrived 15 minutes late to the session and slouched in the chair.
The components of a soap note are easy to remember because soap is a mnemonic that uses all of the letters of soap. Vital signs examination results lab results patients measurements and age. Consider these tips as you do write. Tips on writing a soap note having gone through the basic facts of the components of soap note here are some brief tips on how to develop an excellent soap note.
Tips on writing a soap notes to make the briefing note effective follow the format. This area shows what is going to happen from this point forward with a patientie medications prescribed labs ordered referrals. Make sure you follow the prescribed format you soap note should start from the subjective and then the objective followed by the assessment and conclude with the plan. This part contains history and subjective findings.
A stands for assessment diagnosis. To write a soap note start with a section that outlines the patients symptoms and medical history which will be the subjective portion of the note.

























.jpg)